Gorilla Glue ingestion in dogs: 22 cases (2005–2019)

From the May/Jun 2021 issue. Subscribe today to get your copy
Sarah Friday, DVM, Christina Murphy, DVM, Daniel Lopez, DVM, DACVS, Philipp Mayhew, DVM&S, DACVS, David Holt, BVSc, DACVS
From the Department of Clinical Studies, Matthew J. Ryan Veterinary Hos-pital at the University of Pennsylvania, Philadelphia, Pennsylvania (S.F., D.H.); MSPCA-Angell Animal Medical Center, Boston, Massachusetts (C.M.); Department of Clinical Sciences, College of Veterinary Medicine, Cornell University, Ithaca, New York (D.L.); and Department of Surgical & Radiological Sciences, UC Davis Veterinary Medicine, Davis, California (P.M.).
Correspondence: [email protected] (S.F.)
Accepted for publication: September 29, 2020.
MDI (methylene diphenyl diisocyanate)
ABSTRACT
Gorilla Glue contains methylene diphenyl diisocyanate that expands significantly and hardens once exposed to moisture. Case reports of methylene diphenyl diisocyanate glue ingestion in dogs document gastrointestinal foreign body formation and mechanical obstruction. Medical record queries from four veterinary hospitals identified 22 dogs with Gorilla Glue ingestion. Records were evaluated retrospectively to characterize clinical presentation, diagnostic findings, treatment, and patient outcome. Vomiting was the most common clinical sign (n = 11), with a median time from ingestion to presentation of 42 hr. Abnormal abdominal palpation (e.g., pain) was the most reported examination finding (n = 13). Radiographs were performed in 18/22 dogs, with Gorilla Glue expansion described as granular or mottled soft tissue with gas in the stomach. In 73% (11/15) of dogs requiring surgery, history, clinical findings, and survey abdominal radiographs sufficed to proceed with celiotomy. Surgical removal of the Gorilla Glue foreign body was performed via gastrotomy (n = 14) or gastrotomy and duodenotomy (n = 1). Endoscopic removal was performed in one dog. One dog with suspected mechanical obstruction was euthanized owing to financial constraints. Remaining cases were managed conservatively (n = 5). Short-term prog-nosis following appropriate fluid therapy and surgical or endoscopic removal was very good. (J Am Anim Hosp Assoc 2021; 57:3. DOI 10.5326/JAAHA-MS-7126)
Introduction
Gorilla Gluea is a common household industrial wood glue that contains expanding adhesives and has been documented to cause clinical signs after ingestion in the dog.1–3 Ingestion of glues containing methylene diphenyl diisocyanate (MDI), such as Gorilla Glue, in dogs and humans may cause gastrointestinal obstruction necessitating surgical intervention.1–8 Isocyanates absorb surrounding moisture through hygroscopic properties and can expand significantly and harden.4,6,9 The mixture of MDI with water and gastric secretions results in a polymerization reaction that leads to foreign body formation.4 Vapor inhalation and dermal contact of isocyanates can also lead to skin irritation and hypersensitivity reactions (e.g., bronchial asthma, pneumonitis), although these pathologic consequences ap-pear to be more common and significant in humans with routine work-related exposures than in veterinary patients.10–12
To date, 4 cases of wood glue or Gorilla Glue ingestion have been reported; another 14 were briefly described after review of the American Society for the Prevention of Cruelty to Animals Animal Poison Control Database from 1998 to 2001.1–3 Exposure occurs after chewing on glue bottles or ingesting spilled bottle contents.2 Poly-urethane glue expansion begins within minutes of ingestion and can reach up to eight times the initial volume of glue ingested.4
Ingestion of as little as 0.5 oz has been documented to yield a foreign body large enough to cause gastrointestinal obstruction.6
Approximately two-thirds of the 18 previously reported cases required a gastrotomy for surgical removal of the hardened glue foreign body, with only 1 requiring gastric resection because of mucosal perforation.1–3 Although surgery is the gold standard treatment for obstructed cases, there is a paucity of data on the efficacy of medical management of Gorilla Glue ingestion. Biochemical aberrations and consistent imaging study reports are also relatively sparse. The aim of this retrospective case series is to document the signalment, presentation, diagnosis, treatment, and outcome of dogs with Gorilla Glue ingestion presented to several referral hospitals.
Materials and Methods
Medical records of dogs diagnosed and treated for Gorilla Glue ingestion that presented to the Ryan Veterinary Hospital of the University of Pennsylvania, Cornell University Hospital for Animals, University of California Davis Veterinary Medical Teaching Hospital, and Angell Animal Medical Center were evaluated between February 2005 and May 2019 retrospectively. Cases were included regardless of intervention type (i.e., conservative/medical, surgical, endoscopic). Cases were excluded if Gorilla Glue ingestion was suspected by the owner but no physical or radiographic evidence of ingestion was found.
Data retrieved from the medical records included patient signalment, time from glue exposure to presentation (if known), whether glue ingestion was witnessed, presenting complaint, physical examination abnormalities, blood work performed, hematologic and biochemical abnormalities, imaging performed, whether surgical or endoscopic removal was necessary, surgery or endoscopic findings and treatment, postoperative complications, and outcome.
For the time from exposure, cases noted to have ingested glue with the qualitative description of “previous evening” were assigned a time of 24 hours. If a time range was provided (e.g., 2–3 days), the range was averaged (e.g., 2.5 days). Blood work abnormalities were determined in accordance with published canine reference bio-chemical and hematologic values.13 Radiographic and/or ultrasonographic reports from a boarded radiologist were included when available. The surgical and endoscopic findings noted included the size of the glue foreign body, site of the partial or complete mechanical obstruction, gastrointestinal mucosal integrity, treatment (i.e., gastrotomy, enterotomy, or endoscopic removal), and incision size. Long-term patient follow-up was obtained via information available in the hospital medical record. Owners were contacted for the dogs who were managed as outpatients. Three contact attempts were made before the case was considered lost to follow-up. Cases without follow-up were included for information on signalment and presentation.
Statistical analysis was not performed owing to the descriptive nature of the study. All quantitative data were therefore reported as median, as the normality of distribution was not determined.
Results
Twenty-two dogs representing 12 different breeds met the selection criteria from the four participating veterinary referral hospitals. Mixed breeds were most common (n = 11); other breeds included were the French bulldog, Labrador retriever, American pit bull terrier, rottweiler, English mastiff, boxer, Rhodesian ridgeback, cocker spaniel, Great Dane, border collie, and Saint Bernard (n = 1 each). The median patient age was 1 yr with a range of 0.41–8.5 yr. Median weight was 24.5 kg, ranging from 4.4 to 81 kg. Within the patient population, there were 12 females (9 spayed, 3 intact) and 10 males (8 castrated, 2 intact).
All cases (n = 22) were presented to the emergency room following witnessed Gorilla Glue ingestion by the owner, a history of chewed glue bottle remnants found in the home, or glue residue on the patient’s hair coat. Clinical signs included vomiting (n = 11), inappetence (n = 3), polydipsia (n = 1), and weight loss (n = 1). The approximate time from glue ingestion to presentation ranged from < 1hr to 1008 hr, with a median of 36 hr (n= 21). One dog had an unknown exposure time. The amount of Gorilla Glue ingested was provided in only two medical records, with estimated ingestions of 0.5–1 oz. Other known or suspected ingestion amounts were difficult to quantify owing to inability to determine if leakage from the container, ingestion, or previous usage was responsible for the missing contents.
TABLE 1 Summary Data from 22 Cases Following Gorilla Glue Ingestion
| Case No. | Time from Exposure, hr | Clinical Signs | Abdominal Palpation | Blood Work Abnormalities | Imaging Findings | Treatment/Outcome |
| 1 | Unknown | None reported | Tense | iCa 1.08 mmol/L, PCV 56% | AXR: gastric foreign material consistent with GG | Gastrotomy, recovered |
| 2 | 1.5 | None reported | Painful | TS 6.2 g/dL | XR: gastric foreign material vs. ingesta | Gastrotomy, duodenotomy, recovered |
| 3 | 60 | None reported | Distended | Na 139.4 mmol/L, iCa 1.08 mmol/L, TS 4.8 g/dL | AXR: report NA | Gastrotomy, gastric ulcerations, recovered |
| 4 | 504 | Vomiting | Painful, hard mass | TS 5 g/dL | AXR: report NA | Gastrotomy, recovered |
| 5 | 48 | Vomiting, inappetence | Painful, “full” | iCa 1.13 mmol/L | AXR: report NA | Gastrotomy, recovered |
| 6 | 192 | Vomiting, inappetence | NSF | BE 5.7 mmol/L | NP | Gastrotomy, recovered |
| 7 | 168 | Vomiting, inappetence | Pain, mass in cranial abdomen | NSF | NP | Gastrotomy, no follow-up |
| 8 | 7 | None | NSF | PCV 56%, lactate 3.5 mmol/L | AXR: report NA | Gastrotomy, no follow-up |
| 9 | <12 | None | NSF | NP | AXR: report NA | Gastrotomy, recovered |
| 10 | 12 | Vomiting | Tense, painful | K 3.58 mmol/L, iCa 1.39 mmol/L, lactate 7.8 mmol/L | AXR: stomach contains granular soft tissue material | Gastrotomy, gastric mucosa erythematous, recovered |
| 11 | 48 | Vomiting | NSF | NP | AXR: granular material in stomach | Gastrotomy, recovered |
| 12 | 24 | Vomiting | “Full” | NP | AXR: large amount of heterogeneous gastric material, small intestine diffusely gas filled | Gastrotomy, recovered |
| 13 | 1008 | Vomiting, weight loss | Large mass | NP | AXR: gastric distension with soft tissue opaque material; AUS: stomach markedly distended with hyperechoic shadowing object | Gastrotomy, recovered |
| 14 | 48 | Vomiting | NSF | iCa 1.36 mmol/L | AXR: space filling gastric opacity; AUS: moveable mass in stomach; Gastroscopy: GG FB in pyloric antrum | Gastrotomy, recovered |
| 15 | 36 | Vomiting | Enlarged stomach | Na 138.7 mmol/L, K 3.34 mmol/L, Cl 93 mmol/L, PCV 56% | AXR: grossly distended stomach, obstructive pattern at pylorus | Gastrotomy, mild mucosal ulceration, febrile 5 days postoperative |
| 16 | 168 | Vomiting | Pain | NSF | AXR: report NA; focal AUS (fasted): moderate gas, shadowing object in stomach | Endoscopy, moderate mucosal ulceration of LES after removal, recovered |
| 17 | <1 | None | NSF | NP | AXR: NSF | No treatment |
| 18 | 4 | None | NSF | TS 6.2 g/dL | AXR: ingesta vs. GG in stomach | No treatment, foreign material passed next day (per owner follow-up) |
| 19 | 4 | Vomiting (induced) | NSF | NP | AXR: NSF | Emesis induction before presentation; discharged with gastroprotectants |
| 20 | 1 | None | Tense, painful | TS 6.3 g/dL | AXR: stomach distended with mottled soft tissue opacity, caudal displacement of small intestines | No treatment, no follow-up |
| 21 | 48 | NA | Pain, firm mass, suspect gastrointestinal obstruction | NP | NP | Medical management, no follow-up |
| 22 | 24 | NA | Not specified, but gastrointestinal obstruction suspected | NP | NP | Euthanized |
AUS, abdominal ultrasound; AXR, abdominal radiographs; BE, base excess; FB, foreign body; GG, Gorilla Glue; iCa, ionized calcium; LES, lower esophageal sphincter; NA, records not available; NP, not performed; NSF, no significant findings; PCV, packed cell volume; TS, total solids.
Abnormal abdominal palpation (particularly cranial) was the most frequently reported abnormal physical examination finding. Thirteen of the 22 dogs had one or a combination of the following on abdominal palpation: pain (n = 8), palpable mass (n = 4), tense abdomen (n = 3), “full” cranial abdomen (n = 2), and/or gastric distension (n = 2; Table 1). Three dogs had hardened glue on the muzzle, palate, teeth, or forelimbs. None of these dogs had a palpable abdominal mass. Four dogs were described as depressed or lethargic. Dehydration, hypersalivation, and hyperemic and tacky mucous membranes were less commonly noted in 1 dog each. Four dogs had no significant findings on physical examination; 2 of these dogs required surgical removal of a glue foreign body.
Either blood gas analysis or packed cell volume and total solids were performed in 63.6% of dogs. One dog (No. 6, Table 1) had a mild metabolic alkalosis. Three other dogs had mild to moderate hyponatremia, hypokalemia, and/or hypochloremia. In addition, mild to moderate hyperlactatemia (n = 2), mild to moderate ionized hypocalcemia (n = 3), mild to moderate ionized hypercalcemia (n = 2), mildly increased packed cell volume (n = 3), and low total solids (n = 5) were seen (Table 1).
Eighty-two percent (18/22) of dogs had abdominal radiographs performed either at the primary veterinarian (n = 3) or on admission to the referral hospital (n = 15). The radiology report was unavailable for 6 dogs.
History, clinical findings, and abdominal radiographs were sufficient to proceed with surgery in 11 dogs. In these, radiographic reports described the gastric contents as having a granular soft tissue appearance, mottled soft tissue and gas opacity, or heterogeneous ingesta character (Figure 1). Foreign material was evident as early as 1.5 hr after exposure. Gross gastric distention with a pattern of pyloric obstruction was reported in only one dog (No. 15, Table 1). In two dogs, celiotomy was performed without any abdominal imaging; one (No. 6) had a witnessed Gorilla Glue ingestion 8 days prior and was depressed with hyperemic mucous membranes on presentation, whereas the other dog (No. 7) had a softball-sized mass on abdominal palpation. Abdominal ultrasound was per-formed after abdominal radiographs in three dogs whose radiographs showed equivocal soft tissue opacities (Nos. 13, 14, and 16).
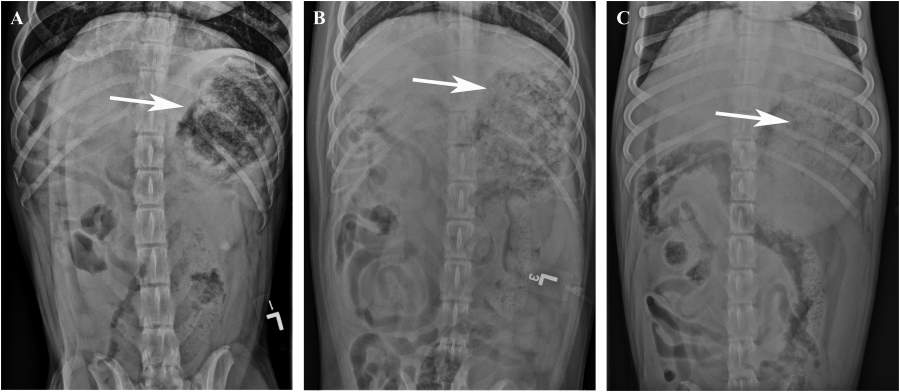
FIGURE 1 Ventrodorsal radiographs showing heterogeneous soft tissue/gas material (white arrows) in the stomach characteristic of a Gorilla Glue foreign body in a (A) 2 yr old female spayed mixed-breed dog (No. 1, Table 1), (B) 1 yr old Labrador retriever (No. 2), and (C) 6 mo old American pit bull terrier (No. 18).
Surgical removal of the Gorilla Glue foreign body was elected in 65.2% (15/23) of dogs via gastrotomy alone (n = 14) or gastrotomy and duodenotomy (n = 1). The size of the glue foreign body ranged from 5–6 cm in diameter to 15 × 15 × 25 cm and was described as spongy to hard in consistency (Figure 2). All gastrotomy incision lengths were reported to be within 2 cm of the smallest dimension of the foreign body. In the dog requiring a duodenotomy (No. 2, Table 1), an ~8 cm piece of glue foreign body was removed through the enterotomy site and an orogastric tube was passed to facilitate removal of the remaining small pieces of glue via lavage and gastric massage. Surgery reports were unavailable for two dogs. The size of the glue foreign body was not described in five dogs, in whom the gastrotomies were described as straightforward or routine.
Endoscopic removal of the Gorilla Glue foreign body was performed in one dog (No. 16, Table 1). A large solid mass of glue was observed in the gastric fundus measuring ~8 × 4 cm that was able to be cut with a snare and removed in multiple smaller pieces. Two remaining fragments estimated to be 4 mm in diameter were left to be passed.
Several small (< 1 cm) mucosal ulcerations were noted in one gastrotomy, and the gastric mucosa was noted to be slightly erythematous in three other gastrotomy cases. The dog who underwent endoscopic glue removal had diffuse multifocal petechiation and moderately erythematous gastric mucosa. Excessive mucosal injury or gastrointestinal perforation necessitating gastric or intestinal resection was not reported in any surgical cases. Perioperative treatment included IV fluids, antacids (famotidine, omeprazole), antiemetics (ondansetron), and analgesics (tramadol).
Surgery or endoscopy was not performed in six dogs (Nos. 17–22 in order described, Table 1). The first dog only had glue evident on the hard palate and muzzle with no evidence of foreign material on abdominal radiographs and so was discharged without treatment. The second had granular soft tissue material within the gastrointestinal tract on survey abdominal radiographs that was not apparent on repeated radiographs the following day. Emesis was induced with hydrogen peroxide by the owner of one dog 10 min after glue ingestion. The dog was bright and alert on presentation with no significant findings on examination or abdominal radiographs and was discharged. Outpatient management was elected in two dogs, one of whom had abdominal radiographs with no obstructive pattern and material indistinguishable between ingesta and Gorilla Glue. Mechanical obstruction was suspected in the second dog based on the depressed physical status and firm structure on abdominal palpation. Subcutaneous fluids, chlorpromazine, and analgesics (unspecified) were administered before discharge. The dog was discharged with recommendations for an expedient recheck with the primary veterinarian the next day. Both dogs were lost to follow-up. The final dog had suspected mechanical obstruction secondary to witnessed Gorilla Glue ingestion and was humanely euthanized owing to financial constraints.
One dog (No. 15, Table 1) treated with a gastrotomy re-presented 5 days postoperatively with pyrexia and had an abdominal effusion containing cocci when evaluated by the referring veterinarian. The dog was febrile on presentation to the referral institution but showed no evidence of free abdominal fluid on abdominal ultrasound. Cephalexin was prescribed and no further follow-up was available. Aside from this dog, no immediate post-operative complications were reported. Three dogs had hospital visits documented 4–8 yr following surgical management for un-related ailments. Long-term patient outcome data were unavailable for the remaining surgical cases.
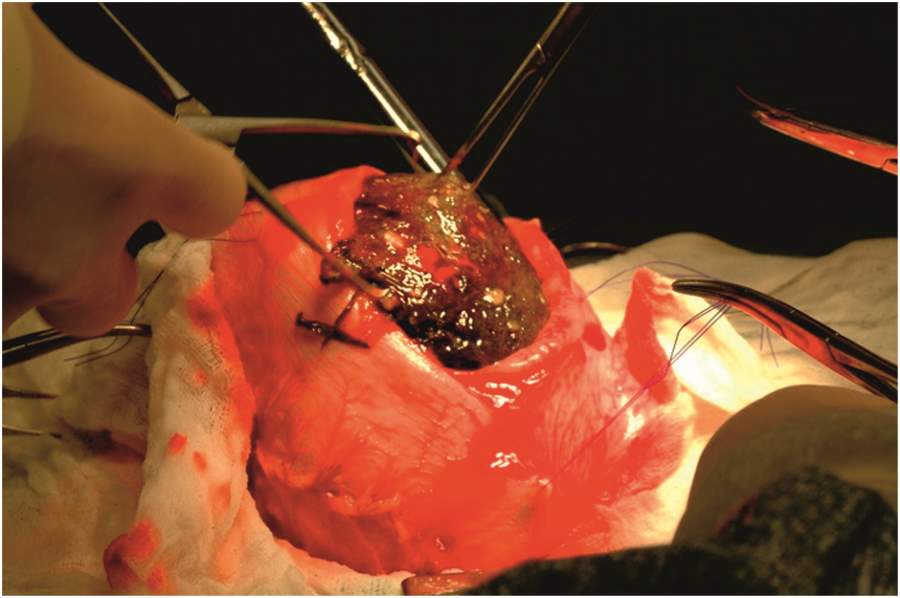
FIGURE 2 Intraoperative photograph of the Gorilla Glue foreign body to be removed through the gastrotomy.
Discussion
The findings of this study suggest that Gorilla Glue gastrointestinal foreign bodies in dogs are relatively uncommon considering the frequency with which other types of gastrointestinal foreign bodies are encountered in primary and referral veterinary practices.14 Only 22 cases of Gorilla Glue ingestion were seen over a 15 yr period within four large referral hospitals.
Our patient population was mostly young, medium- to large-breed dogs. This signalment is similar to those reported in retrospective studies of other gastrointestinal foreign bodies, possibly because younger dogs are more prone to dietary indiscretion.15 Similar to existing case reports of Gorilla Glue and other foreign body ingestions, vomiting, inappetence, and abdominal pain were among the most common clinical signs.2–4,14,16
Acid–base and electrolyte abnormalities are commonly encountered in animals with gastrointestinal disease, particularly in cases of mechanical obstruction in which electrolyte secretion and absorption, fluid balance, and acid–base dynamics are altered both proximal and distal to the obstruction site.15,17 Subsequent vomiting and inappetence further derange electrolytes and acid–base status. Regardless of the site of gastrointestinal obstruction, hypochloremia, metabolic alkalosis, hyperlactatemia, hypokalemia, and hyponatremia are the most common acid–base and electrolyte abnormalities according to one retrospective study of 138 dogs with gastrointestinal foreign bodies.15 Interestingly, these changes were not commonly found in the current study. It is not clear if there are any metabolic consequences from the interaction of MDI with saliva, gastric acid, and water. Of the 12 cases in which blood gas analyses were performed, only 4 had one or more electrolyte or acid–base abnormalities. More commonly, hyperlactatemia, low total solids, and ionized hypocalcemia were found. Hyperlactatemia was noted by Boag and others in ~40% of gastrointestinal foreign bodies.15 Intestinal ischemia was not likely as a contributing factor, as this was not observed intraoperatively.
Client history, clinical signs, and survey abdominal radiographs diagnosed a Gorilla Glue foreign body in most dogs. This appears to be the appropriate diagnostic approach for the majority of Gorilla Glue ingestion cases. Abdominal ultrasound (n = 3) and gastroscopy (n = 2) were additional imaging modalities used in a small number of cases. All surgical cases in the current study had gastric foreign bodies. The imaging modality of choice for definitive diagnosis of gastric foreign bodies is somewhat controversial. Ninety-five percent of gastric foreign bodies were visible on survey abdominal radiographs in one study.18 The current study reports lower detection rates (73%) for Gorilla Glue, perhaps because it does not retain its shape upon ingestion, but rather fills potential space. The radio-graphic appearance of expanded Gorilla Glue within the stomach was often described as having a mottled soft tissue and gas opacity. The polymerized substance is radiopaque, aiding in radiographic detection, but there are radiographic similarities in the appearance of Gorilla Glue and undigested kibble. Food engorgement may have very similar clinical presentation and appearance on radiographs, necessitating thorough history-taking.19 Radiographically differentiating food engorgement from Gorilla Glue ingestion may be difficult. Food should digest and empty from the stomach, whereas polymerized MDI would remain, so repeating abdominal radio-graphs several hours after an initial radiographic study may be of benefit. Neither pneumogastrography nor positive contrast studies were used in the current study, but the clinical utility of these techniques has been documented in the diagnosis of soft tissue foreign bodies (e.g., string, grass, fabric), as well as mural gastric lesions.20 It is possible that these techniques may prove useful in differentiating glue foreign bodies from ingesta, as contrast medium may outline pieces of ingesta and coat a solid glue mass. Contrast studies may be efficacious in a primary practice setting where ultrasound and gastroscopy are unavailable or cost prohibitive. Abdominal ultrasonography is potentially limited by the presence of gas within the stomach, cost, and operator experience, and provided diagnostic clarity in only one case in the current study.21
The surgical removal of the Gorilla Glue foreign material appeared routine and similar across the surgical reports for all 15 cases. The decision to perform surgery was likely clinician dependent and probably based on clinical experience, the perceived size of the foreign body, and owner finances. The proximal location of the foreign body within the stomach is attributed to the size of the foreign body, preventing movement through the pylorus in all but one case. This is consistent with the foreign body location in previous case reports.1–3 Although MDI glue does not adhere to the mucosal surface upon ingestion, it can cause congestion, laceration, and, rarely, bowel perforation.4 Despite the chronicity of the foreign bodies (up to 6 wk in one case) and severe gastric distension secondary to glue expansion in some cases, the mucosa was noted to be intact in all surgical cases in the present study. Small mucosal ulcerations were the most severe gastric pathology documented. Ulcerations may have been associated with heat or urea production from polymerization4 or mechanical abrasion.22,23 Gastric resection was not required in any case.
One of the 15 dogs treated surgically had a documented postoperative complication of pyrexia; bacteria were seen on abdominal effusion cytology during evaluation by the primary veterinarian. The presence of toxic neutrophils and intracellular bacteria in peritoneal fluid in animals with pyrexia and other compatible clinical signs raise concerns for peritonitis in animals who have had recent gastrointestinal surgery. However, bacteria may be present in the abdominal fluid of dogs with uneventful recoveries following celiotomy.23–25 No free abdominal fluid was seen at the referral hospital so a diagnosis of septic peritonitis could not be confirmed.
This series includes the first documented case of successful endoscopic removal of a Gorilla Glue foreign body from a dog. The foreign body size (~8 × 4 cm) was not significantly smaller than some of those that were surgically removed. The material could be broken into smaller, removable pieces, even though it had been in the stomach for an estimated 7 days. It is possible that more cases would have been amenable to endoscopic removal had this technique been attempted. The chronicity of foreign glue material within the gastrointestinal tract does not appear to prevent frag-mentation during endoscopy.
This study has several limitations because it was retrospective. Standard data were not collected from all four participating hospitals. The records also do not indicate the time from ingestion to onset of clinical signs, which could have important treatment implications. Outpatient management following Gorilla Glue ingestion was not as well represented in our case series. Unfortunately, follow-up was only available for one of the three cases (Nos. 18, 20, and 21, Table 1) in which supportive care and monitoring was elected. Induction of emesis following Gorilla Glue ingestion was reported as successful in one case with no short-term complications.11 However, this approach is generally contraindicated.4 Polymerization of MDI occurs within minutes.4 Larger polymerized masses are unlikely to move out of the stomach and smaller masses may become esophageal foreign bodies. The potential for aspiration pneumonia is also a concern. Surgical removal via gastrotomy is a procedure that is relatively straightforward and accessible to the majority of general practitioners.
Conclusion
Gorilla Glue ingestion is relatively uncommon in dogs but can lead to foreign body formation and gastric outflow obstruction following glue polymerization. A thorough client history, abdominal palpation, and survey abdominal radiographs are often adequate to make the diagnosis. The glue foreign body is usually contained within the stomach and, in the present case series, was not associated with persistent clinical signs of mucosal injury. Patients receiving fluid therapy and gastrotomy demonstrated a very good short-term outcome.
FOOTNOTES
a Gorilla Glue; The Gorilla Glue Company, Cincinnati, Ohio
REFERENCES
1. Lubich C, Mruos R, Krenzelok EP. Beware of canine Gorilla Glue in-gestions. Vet Hum Toxicol 2004;46:153–4.
2. Horstman CL, Eubig PA, Khan SA, et al. Gastric outflow obstruction after ingestion of wood glue in a dog. J Am Anim Hosp Assoc 2003;39: 47–51.
3. Bailey T. Toxicology brief: the expanding threat of polyurethane adhesive ingestion. Vet Tech 2004;25:426–8.
4. Fitzgerald KT, Bronstein AC. Polyurethane adhesive ingestion. Top Companion Anim Med<e/m> 2013;28:28–31.
5. Tanimu S, Williams C, Onitilo AA. Small-bowel obstruction from Gorilla Glue ingestion. Gastrointest Endosc<e/m> 2019;90(2):308–9.
6. Peterson KL. Glues/adhesives. In: Osweiler GD, Hovda LR, Brutlag AG, et al., eds. Small animal toxicology. Ames (IA): Wiley; 2011:89–95.
7. Gwaltney-Brant SM. Miscellaneous indoor toxicants. In: Peterson ME, Talcott PA, eds. Small animal toxicology. 3rd ed. St. Louis: Elsevier; 2013: 291–308.
8. Goertemoeller SI, Sweeny RM. Unique foreign body ingestions in the pediatric population. J Emerg Nurs 2010;36(2):178–9.
9. ISOPA. Safety information: Properties, Hazards and Safety information for MDI. Available at: http://www.isopa.org. Accessed November 5, 2019.
10. Yamada K, Amitani R, Miimi A, et al. Interstitial pneumonitis-like lesions in guinea-pigs following repeated exposure to toluene diisocyanate. Eur Respir J 1995;8:1300–6.
11. Lemiére C, Romeo P, Chaboillez S, et al. Airway inflammation and functional changes after exposure to different concentrations of isocyanates. J Allergy Clin Immunol 2002;110(4):641–6.
12. Musk AW, Peters JM, Wegman DH. Isocyanates and respiratory disease: current status. Am J Ind Med 1988;13:331–49.
13. Jacobs RM, Lumsden JH, Taylor JA. Canine and feline reference values. In: Bonagura JD, ed. Kirk’s current veterinary therapy XIII. Philadelphia: WB Saunders; 2000:1207–27.
14.Aronson LR, Brockman DJ, Brown DC. Gastrointestinal emergencies. Vet Clin North Am Small Anim Pract 2000;30(3):555–79.
15. Boag AK, Coe RJ, Martinez TA, et al. Acid-base and electrolyte abnor-malities in dogs with gastrointestinal foreign bodies. J Vet Intern Med 2005;19:816–21.
16. Hayes G. Gastrointestinal foreign bodies in dogs and cats: a retrospective study of 208 cases. J Small Anim Pract 2009;50:576–83.
17. Shields R. The absorption and secretion of fluid and electrolytes by the obstructed bowel. Br J Surg 1965;52:774–9.
18. Gianella P, Pfammatter NS, Burgener IA. Oesophageal and gastric endoscopic foreign body removal: complications and follow-up of 102 dogs. J Small Anim Pract 2009;50:649–54.
19. Smart L, Reese S, Hosgood G. Food engorgement in 35 dogs (2009-2013) compared with 36 dogs with gastric dilation and volvulus. Vet Rec 2017; 181(21):563–9.
20. Bowlus RA, Biller DS, Armbrust LJ, et al. Clinical utility of pneumogastrography in dogs. J Am Anim Hosp Assoc 2005;41:171–8.
21. Tyrrell D, Beck C. Survey of the use of radiography vs. ultrasonography in the investigation of gastrointestinal foreign bodies in small animals. Vet Radiol Ultrasound 2006;47:404–8.
22. Amorim I, Taulexcu MA, Day MJ, et al. Canine gastric pathology: a review. J Comp Pathol 2016;154:9–37.
23. Botte RJ, Rosin E. Cytology of peritoneal effusion following intestinal anastomosis and experimental peritonitis. Vet Surg 1983;12(1):20–3.
24. Szabo SD, Jermyn K, Neel J, et al. Evaluation of postceliotomy peritoneal drain fluid volume, cytology, and blood-to-peritoneal fluid lactate and glucose differences in normal dogs. Vet Surg 2011;40(4):444–9.
25. Guieu LS, Bersenas AM, Brisson BA, et al. Evaluation of peripheral blood and abdominal fluid variables as predictors of intestinal surgical site failure in dogs with septic peritonitis following celiotomy and the placement of closed-suction abdominal drains. J Am Vet Med Assoc 2016; 249(5):515–25.



